

In HPV-driven OPSCC surveillance

*Of 1,076 patients tested during surveillance, 80 (7.4%) had at least one positive TTMV-HPV DNA Score. Of these, 59 (74%) had either indeterminant (IND) disease status or no evidence of disease (NED) at time of their positive test Score, while 21 (26%) were noted as having clinically active disease at time of their first positive Score. Nearly half, 38 (48%) were tested >12 months after completion of definitive therapy, while 27 (34%) and 15 (19%) were tested at 6-12 months, and 3-6 months, respectively.
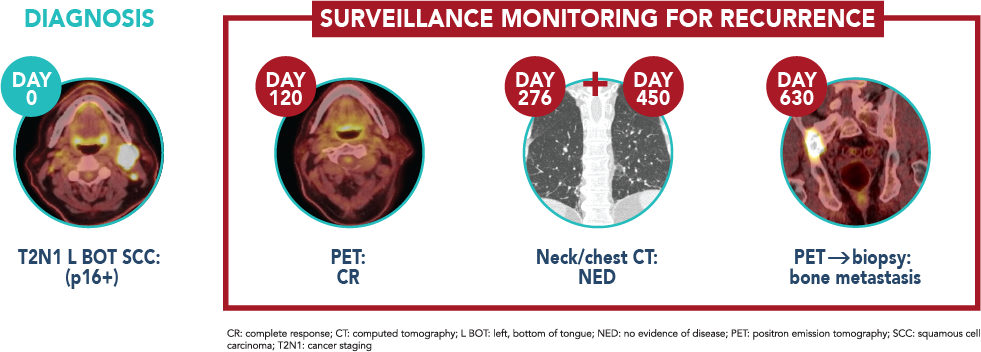
†57 of the 59 (96.66%) patients with IND or NED status, who tested positive for TTMV-HPV DNA, were later proven to have recurrent disease (on imaging and/or biopsy), suggesting the presence of clinically occult recurrence at time of their positive test result. Longer follow-up was needed to identify recurrent cancer in 2 of the remaining 4 IND and NED patients under surveillance. All 21 patients with active disease reported at the time of TTMV-HPV DNA testing were confirmed to have recurrent disease.
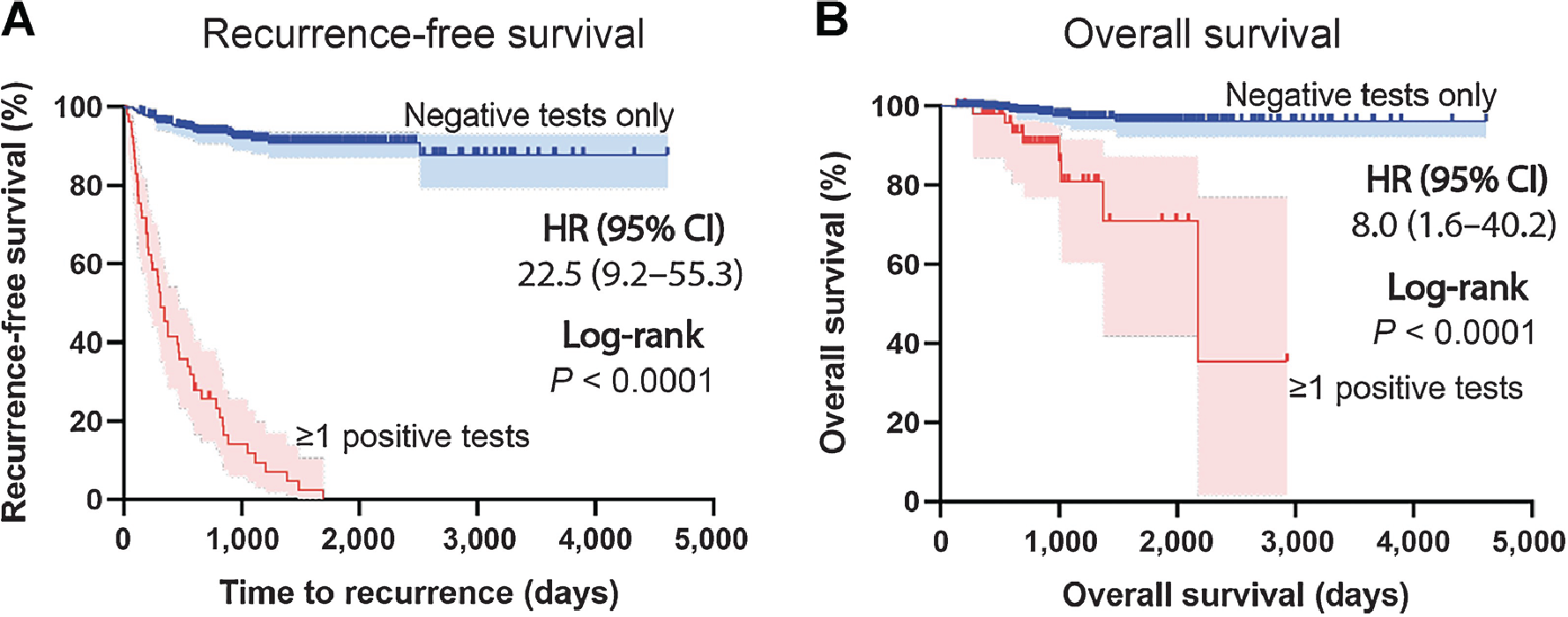
‡Survival among HPV-associated oropharyngeal cancer survivors based on surveillance TTMV-HPV DNA test results. Recurrence-free survival (A) and overall survival (B) curves separated by patients in the entire study cohort with negative surveillance TTMV-HPV DNA results vs. those with a positive TTMV-HPV DNA test result at any timepoint during surveillance; Kaplan–Meier method; log-rank testing (two-sided),
 ≤2 years post treatment: every 3 months
≤2 years post treatment: every 3 months
 3-5 years post treatment: every 6 months
3-5 years post treatment: every 6 months
 6+ years post treatment: 1 time per year
6+ years post treatment: 1 time per year
References
1. Ferrandino RN, Chen S, Kappauf C, et al. Performance of liquid biopsy for diagnosis and surveillance of human papillomavirus–associated oropharyngeal cancer. JAMA Otolaryngol Head Neck Surg. doi:10.1001/jamaoto.2023.1937. 2. Hanna GJ, Roof SA, Jabalee J, et al. Negative predictive value of circulating tumor tissue modified viral (TTMV)-HPV DNA for HPV-driven oropharyngeal cancer surveillance. Clin Cancer Res 2023. doi: 10.1158/1078-0432.CCR-23-1478. 3. Berger BM, Hanna GJ et al. Detection of Occult Recurrence Using Circulating Tumor Tissue Modified Viral HPV DNA among Patients Treated for HPV-Driven Oropharyngeal Carcinoma. Clin Cancer Res 2022;28(19):4292–4301. 4. Chera BS, Kumar S, Shen C, et al. Plasma circulating tumor HPV DNA for the surveillance of cancer recurrence in HPV-associated oropharyngeal cancer. J Clin Oncol. Apr 1 2020;38(10):1050-1058. doi:10.1200/JCO.19.02444. 5. Lin MG, Zhu A, Read PW, et al. Novel HPV associated oropharyngeal squamous cell carcinoma surveillance DNA assay cost analysis. Laryngoscope. Nov 2023; 133:306-312. 6. Chera BS, Kumar S, Beaty BT, et al. Rapid clearance profile of plasma circulating tumor HPV type 16 DNA during chemoradiotherapy correlates with disease control in HPV-associated oropharyngeal cancer. Clin Cancer Res. Aug 1 2019;25(15):4682-4690. doi:10.1158/1078-0432.CCR-19-0211 7. International Agency for Research on Cancer. Human papillomaviruses. IARC monographs on the evaluation of carcinogenic risks to humans. Volume 90. Geneva, Switzerland: World Health Organization, 2007. 8. Mijares K, Ferrandino R, Chai R, et al. Circulating Tumor HPV DNA in Patients With Heand and Neck Carcinoma: Correlation With HPV Genotyping. Am J Surg Pathol. 2023:00:000-000. 9. Mirghani H, Moreau F, Lefevre M, et al. Human papillomavirus type 16 oropharyngeal cancers in lymph nodes as a marker of metastases. Arch Otolaryngol Head Neck Surg. Sep 2011;137(9):910-4. doi:10.1001/archoto.2011.141. 10. Gupta T, Master Z, Kannan S, et al. Diagnostic perfor¬mance of post-treatment FDG PET or FDG PET/CT imaging in head and neck cancer: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging38, 2083–2095(2011). doi.org/10.1007/s00259-011-1893-y. 11. Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. Jul 1 2010;363(1):24-35. doi:10.1056/NEJMoa0912217 12. Fakhry C, Zhang Q, Nguyen-Tan PF, et al. Human papillomavirus and overall survival after progression of oropharyngeal squamous cell carcinoma. J Clin Oncol. Oct 20 2014;32(30):3365-73. doi:10.1200/JCO.2014.55.1937 13. Gillison ML, Trotti AM, Harris J, et al. Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): a randomised, multicentre, non-inferiority trial. Lancet. Jan 5 2019;393(10166):40-50. doi:10.1016/S0140-6736(18)32779-X. 14. Elaldi R, Roussel LM, Gal J, et al. Correlations between long-term quality of life and patient needs and concerns following head and neck cancer treatment and the impact of psychological distress. A multicentric cross-sectional study. Eur Arch Otorhinolaryngol. Jul 2021;278(7):2437-2445. doi:10.1007/s00405-020-06326-8. 15. Kuhs KA, Brenner CJ, Holsinger CF, et al. Circulating tumor HPV DNA for surveillance of HPV-positive oropharyngeal squamous cell carcinoma, JAMA Oncol. doi:10.1001/jamaoncol.2023.4042. Published online October 12, 2023.
about how the NavDx test is helping
optimize HPV-driven cancer care
This site is protected by reCAPTCHA and the Google Privacy
Policy.
Terms of Service apply.
about how the NavDx test is helping
optimize HPV-driven cancer care
This site is protected by reCAPTCHA and the Google Privacy Policy.
Terms of Service apply.